Claudia De Pasquale makes herself whole with reconstruction choices
- 02/17/26

At 40, I was the picture of health — or so I thought. My days were a blur of lunchboxes, carpools, and bedtime stories. My routine mammogram had just come back clear, though someone noted my breasts were “extremely dense.” I didn’t think much about it; I had three kids and no time for Dr. Google
One year later, during my annual OB-GYN check, my doctor paused mid-exam and said, “Hmm.” Nobody wants to hear a “Hmm.” Biopsies soon revealed multifocal invasive lobular carcinoma — a sneaky breast cancer that often hides from mammograms. Suddenly, I was thrust from soccer fields and school pickups into scans, surgery, and survival mode.
So many decisions, so few real answers
After my mastectomy of the affected breast, I faced another huge decision: breast reconstruction. My first plastic surgeon assumed I wanted an “upgrade.” He even overfilled my tissue expander — a temporary expandable implant until my full reconstruction — aiming for a DD size I never asked for. At that point I had one breast stretched and ballooned — and on my other side, the one that had nursed three babies, sagging naturally. It was painful and jarring. I hated looking in the mirror. I couldn’t even wear a normal bra; nothing fit.
And when that realization finally came, so did the certainty: This was not my surgeon.
I hated the expander — that hard, foreign object sitting inside me. My chest felt uneven and unnatural, and because I didn’t have much body fat to cushion it, every single ripple and ridge of that expander showed through my skin. It looked and felt wrong — like a hollow reminder of what had been taken away. I had this gaping hole in my chest, and with it, an even bigger one inside me.
Every time I looked in the mirror, I was reminded of cancer and everything it had stripped from my body and sense of self. It wasn’t just physical discomfort; it was emotional pain, too. I was tired of hospitals, tired of being the patient, tired of pretending I was fine for everyone else.
I also understood that replacing the expander with implants might feel more comfortable initially, but because I didn’t have much fat, rippling would likely remain an issue. Fat grafting could help, but only about half of it typically “sticks,” meaning I might end up needing multiple surgeries just to look and feel the way I wanted. The thought of more operating rooms, more recovery, and still not feeling whole again — I just couldn’t accept that.
New surgeon, more options
Flap surgery was barely mentioned by my plastic surgeon — brushed aside as if it wasn’t really an option — and “going flat” wasn’t discussed at all. It was simply assumed I would want and need implants. I didn’t realize at the time that flap surgery requires advanced microsurgical skill and that many surgeons can’t perform it.
When I found the courage to bring a flap surgery up again, I was told that in my case and of my build (tall and athletic): If you were my wife, get implants; if you were my ex-wife, get a flap. It was meant to be a joke, but to me it was crushing. My body and my future deserved better than punchlines and assumptions.
I was so shocked that I couldn’t even find the words. I remember sitting there on the exam table, staring at my reflection — one side huge and stretched to the point of discomfort, the other soft and familiar. I felt like a stranger in my own body. The surgeon kept talking, saying how busy those microsurgeons were and how they would probably tell me the same thing anyway.
I went home feeling completely drained — hopeless, even. And then the anger set in.
How dare he tell me what I should want? How dare he decide what was right for my body?
But the truth is, I was so worn down from all the treatment — the surgeries, the chemo, the endless appointments, the exhaustion that seeps into your bones — that I didn’t even raise my voice. I just sat there and nodded, too tired to fight.
I didn’t even dare to look in the mirror. I didn’t recognize myself — no hair, no lashes, and now uneven breasts. I looked like Quasimodo. My body had become a project, something to be fixed and reshaped instead of something to heal.
It took a while before I found my voice — but when I did, it came out clear: I don’t want bigger. I don’t want implants. I don’t want foreign objects in my body.
What I wanted was my own tissue, my own skin — a flap. Something real. Something that felt like me.

Discovering flap surgery — and SGAP
I began to meet with several plastic surgeons within my HMO, searching for someone who could help me achieve a natural result using my own tissue. Each consult ended with the same discouraging message: “You are too thin and do not have enough tissue; implants only.” I even began researching out-of-state options. After so many closed doors, I almost gave up.
On to late nights of research and connecting with other survivors. I learned about flap reconstruction — using your own tissue instead of an implant.
When I started researching flap reconstruction, I learned that if my tummy didn’t work — which can happen for women with a more athletic build — there were other options. Women like me had pursued them and succeeded. That gave me hope. It meant I didn’t have to settle for something that didn’t feel right for my body.
I discovered a breast reconstruction center in New Orleans that offered advanced options like the SGAP (superior gluteal artery perforator) flap, which uses tissue from the upper buttocks. Yes, my new breasts came from my butt — something I can laugh about now, but at the time I felt both brave and strange.
Feeling whole again
I started to imagine how I wanted to feel and look in the future — not just next month, but years from now. I pictured myself as a strong, beautiful 60-year-old woman, still active, still vibrant, still me. And then I thought even further — I didn’t want to be a 70-year-old woman with a sagging body but still carrying implants that didn’t match the rest of me. I wanted to stay true to my natural body — to age gracefully, to let time leave its marks honestly, not around something artificial.
It felt like a stretch to think that far ahead — but for the first time since my diagnosis, I allowed myself to dream of growing older. And it suddenly felt so good to carry that image in front of me — that strong, gracefully aging woman who had made it through. It was like a complete reframe: from fear of what might happen to hope for what still could.
Shifting my mindset from short-term fixes to long-term healing changed everything. Yes, it meant choosing a longer, more complicated surgery — but in the long run, it was what I truly wanted.
I am the CEO of my body. I get to choose how I want to look and feel after cancer — not my surgeon, not a statistic, not anyone else.
It wasn’t about perfection anymore. It was about wholeness — about honoring a body that had carried me through cancer and motherhood and still had more life left to live. For the first time since my diagnosis, I could finally imagine what feeling whole again might look like.
And that may look very different for everyone.
It’s about what you want — and listening to that inner voice that suddenly gets very loud when it finally knows what’s right for you.
I am the CEO of my body. I get to choose how I want to look and feel after cancer — not my surgeon, not a statistic, not anyone else.
Planning surgery with kids
Going across the country for a nine-hour surgery with three young kids at home was no small thing. I had to get strategic — and a little creative. So, I did what any mom facing major surgery and chaos would do: I turned into a full-on project manager.
I created color-coded schedules and spreadsheets that could rival a military operation — I planned school drop-offs, after-school activities, playdates, and even dog walks. My amazing friends pitched in for childcare like pros. One of my dearest friends, who worked full time, even stayed at my house so things would keep running smoothly. Another set up a meal train — because nothing says love like dinner magically appearing at your door.
The freezer was stocked with lasagna and chicken nuggets — the official cuisine of survival mode. My friend cooked the kids Spätzle, their favorite dish, and was on speed dial for refills. Thanks to the nonprofit Sharsharet, my kids also got a “busy box” filled with daily surprises so they’d have something to look forward to while I was gone. Honestly, between the gifts, attention, and constant flow of comfort food, I think they had the time of their lives. Nothing like Mom having major surgery to really spice up childhood.
At home, I set up my recovery zone like a mini command center — pillows; wedge cushions; soft, button-down clothes I could actually get on without lifting my arms; drain holders; and a shower chair. My old recliner from my breastfeeding days was moved right by the kitchen — perfect for supervising family life and bossing my husband around while he reheated dinner and tried to remember which kid liked what. Healing, but make it management.
When it was finally time to head to New Orleans, my husband and I left behind the best kind of organized chaos — the kind run by friends who love you enough to juggle your life while you go rebuild your body. At the airport, the kids cried when they said goodbye, and my heart cracked a little. But underneath the emotion was something steady — I knew it would all be OK. I felt confident in my medical team and in this amazing village who would take care of everything back home.
In the weeks leading up to surgery, I used visualization techniques to prepare myself — listening to guided meditations over and over until they became second nature. Each time, I pictured myself calm, safe, and healing. By the time surgery day came, I wasn’t ruled by fear anymore. I felt ready, grounded. Like my body, my mind, and my support system were all finally on the same team.


Why recliners are magical
The surgery itself lasted nine hours. My surgeons checked blood flow with Dopplers every hour that first night — the soft beeping became my lullaby. My husband, my rock, slept on a Murphy bed in the hospital room, ready with ice chips, encouragement, and bad jokes on demand.
Back at home, recovery was no joke. The first three weeks were hard — pain, swelling, exhaustion, and moments of wondering if I’d made a terrible mistake. The first time I saw myself, I was completely blue from bruising, with large scars stretching across my body. My kids were shocked, too — drains hung from my sides, like the arms of an octopus, and I tried to calm them down with a forced smile, saying, “It’s OK — this is just a season. It won’t last.”
That became my daily affirmation: This is just a season. It won’t last. Just like chemo. Just like my mastectomy.
I’m not going to lie — it was much harder than I expected. I’d always considered myself fit and athletic — well, a little less after chemo, but still in good shape. Yet now, I needed help just to get in and out of bed or into a car. Taking a shower felt like a marathon, and the plane ride home was torture. I looked like I’d been run over by a truck.
One night, I completely broke down — full sobs, all the pain and fear catching up with me. My husband reminded me gently, “This is just a season. You’ve been through so much — you’ll get through this, too.” And somehow, I knew he was right.
My recliner — the same one I’d used to breastfeed my three kids — became my throne. I ate there, napped there, scrolled there, and ruled the house from it. Recliners really are magical. I went back and forth between my throne and my bed with my wedge cushions, shuffling carefully, determined to move a little more each day. Every day I walked a few steps. Every day, a few more.
Around that time, I also connected with another survivor who had the same surgery just a day after mine. We bonded instantly — two strangers stitched together by shared experiences. We texted through pain, encouraging each other when it hurt to move, and when progress felt impossibly slow. Her messages lifted my spirit when I needed it most.
Each day, I got a little stronger — baby steps at first. Some days I cried. Others, I just sat in quiet gratitude for my body, my team, and the incredible village that surrounded me.
After six weeks, things began to change. My body started to feel mine again — warm, soft, natural. For the first time in two years, my chest didn’t hold a foreign, hard object. My love handles were gone, and the stubborn little pockets of fat had been optimally relocated to create two new breasts. My glutes even got a subtle lift — the most efficient makeover ever. My body and I made peace.
I went shopping and liked how I looked — not just in clothes, but naked, too. Over time, my scars softened and faded; three years later, they were barely visible. I mourned the loss of sensation, but I was profoundly grateful. Psychologically, it felt liberating — no more looming reconstructive surgeries, no more “what ifs.” I was done.
For the first time since diagnosis, I wasn’t focused on surviving — I was simply living.
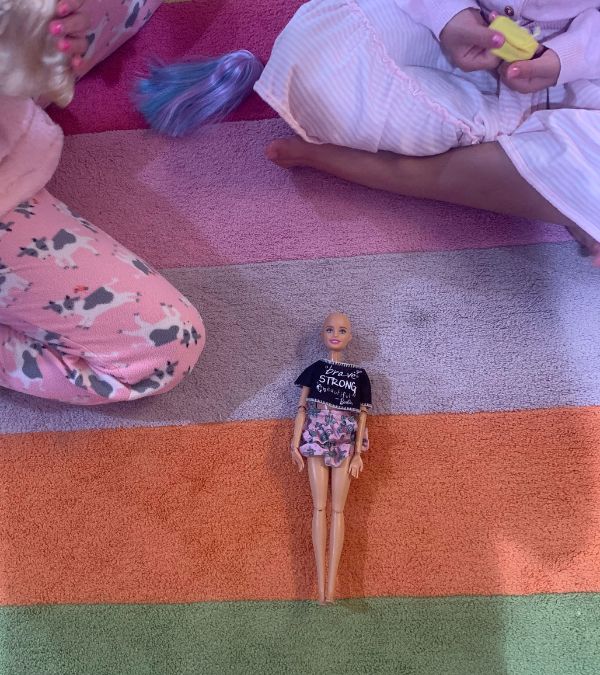
Today, 3 years later, when I look in the mirror, I don’t just see scars; I see resilience and a body that carried me through cancer and back to life. I’m stronger and softer at the same time. My kids see that, too — and I hope they remember that when life hands you something terrifying, you can research, advocate, and choose the path that’s right for you.
Why I share
During my own research, I felt alone and overwhelmed. I wished for a single, honest guide — something with practical tips and the kind of real-life details people don’t always hear in a consult room. That wish became an ebook, Breast Reconstruction: What’s the Deal.
You have choices. It’s not just “implants or nothing.” There are several options — implants, going flat, and different types of flap reconstructions (not just DIEP). Do your research, and research your surgeon even more.
If you’re considering a flap reconstruction, look for a microsurgeon who performs these procedures often — ideally hundreds or even thousands a year. Don’t hesitate to ask for before-and-after photos or to connect with other patients who’ve been through it. The right surgeon will welcome your questions.
You can also choose the timing. Reconstruction doesn’t have to happen at the same time as your mastectomy. You can wait — and sometimes, that’s the better choice if you’re still healing, need additional treatment first, or are navigating insurance coverage. And if your insurance initially denies coverage for the type of reconstruction you want, remember: You have the right to appeal. Many women do — and they succeed.
Advocate for yourself fiercely. Your body, your rules. Ask about your surgeon’s experience with your specific procedure and their flap success rates.
Travel if you need to. Sometimes the right surgeon isn’t nearby, and the trip can be worth it. But not everyone can travel easily — and that’s OK. If distance, cost, or childcare make it difficult, look into organizations and programs that may be able to help.
I often think about how lucky I was to have the support — the friends, childcare, and flexibility — that made my surgery possible. For so many women, travel, time off work, and financial strain can make reconstruction feel out of reach. It shouldn’t be that way. Every woman deserves access to the care and choices that help her feel whole again — whether that means surgery, going flat, or something entirely different.
Build your village. Plan for support like you’re preparing for a new baby — except this time, the baby is you. Lean on family, friends, and community members. Many cancer organizations have resources that can help — ask your patient navigator for guidance.
Kids are resilient. They’ll adapt, help, and make you laugh when you need it most.
If cost feels like a barrier, know that you’re not alone. Insurance is required to cover breast reconstruction under the federal Women’s Health and Cancer Rights Act of 1998 (WHCRA) — though coverage can vary by plan. If you’re worried about costs, talk with your healthcare team. Most cancer centers have financial counselors who can help you navigate coverage and find assistance programs.
And if your claim is denied, you can fight it — and win. The organization Triage Cancer offers excellent free resources to help you understand your rights, appeal insurance denials, and find financial or workplace support.
And remember — it’s OK to ask for financial help. Whether it’s through nonprofits, grant programs, or setting up a personal fundraiser, there are often more options than you realize. Asking doesn’t make you weak — it helps you move forward.
You deserve the option that feels right for you — not the one that’s easiest, cheapest, or most convenient for the system. Advocate for your body, your peace, and your future self.
DISCLAIMER:
The views and opinions of our bloggers represent the views and opinions of the bloggers alone and not those of Living Beyond Breast Cancer. Also understand that Living Beyond Breast Cancer does not medically review any information or content contained on, or distributed through, its blog and therefore does not endorse the accuracy or reliability of any such information or content. Through our blog, we merely seek to give individuals creative freedom to tell their stories. It is not a substitute for professional counseling or medical advice.
Stay connected
Sign up to receive emotional support, medical insight, personal stories, and more, delivered to your inbox weekly.


